Chapter 4
Emerging Microbes
Many infectious diseases, like smallpox, polio, and anthrax, are ancient and have plagued humankind for thousands of years. But new strains of bacteria and viruses continue to emerge seemingly out of nowhere to cause mysterious new ailments.
In Wisconsin in May 2003, three-year-old Schyan Kautzer came down with symptoms vaguely reminiscent of smallpox. Eileen Whitmarsh, a forty-two-yearold pet store owner, developed flulike symptoms along with blisters on her head and under her arms. Two employees at a veterinary clinic also became sick. The one thing they all had in common was a close encounter with prairie dogs. The three-year-old had received a prairie dog for a pet, the pet store owner had had the animals in stock, and the workers at the clinic had recently treated a sick prairie dog.
Blood samples taken from all the victims revealed startling news: They had a disease never encountered before in the Western Hemisphere—a virus called monkeypox, a less severe cousin to smallpox. At one time the virus infected only rodents in Africa, but it had jumped species and was now known to have infected fewer than one hundred people in Africa. But how did it travel five thousand miles across an ocean to a small town in Wisconsin?
A Global Village
Microbes are opportunists. They take advantage of likely and unlikely hosts. The virus that was carried to the United States inside an African rodent seized the opportunity to inhabit a new species when the animal was housed in a small, tightly packed cage next to prairie dogs in a pet store warehouse. The virus mutated, or changed its genetic code, so that it was able to infect a new species. From a Gambian rat to an American prairie dog, it then jumped to a little girl.

Humans live in a global society, and our actions affect the microscopic community around us. "We do things as part of progress, which we don't recognize as changing the microbial environment," 20 says G. Richard Olds, the chairman of medicine at the Medical College of Wisconsin and the former head of the Tropical Disease and Travel Medicine Center in New England. Everything a person does affects the microscopic world: traveling in airplanes, eating foreign foods, and living in crowded cities. As Olds says, "Nothing happens on this planet that doesn't impact us. We're wearing clothes that were made in China. We're eating foods that were grown in Chile." 21 Infective agents can come from anywhere, and frequently do. Monkeypox appeared in this country because of people's passion for exotic pets.
But the connection between man and microbe was not always so apparent. Disease was something that just happened to a person, and there was little thought as to why or how a person's behavior or activities contributed to their illness. It took hundreds of years before someone thought to look at our own behavior and modify it in an attempt to prevent the spread of disease.
The First Disease Detective
In 1854, during the Industrial Revolution, living conditions in many parts of urban England were poor. Factories belched black smoke, and slums were overcrowded and unsanitary—the perfect conditions for bacteria and viruses. An outbreak of cholera occurred in a small area near Broad Street in London. Cholera is contracted by drinking water infected with the cholera bacterium or eating food contaminated by it. Cholera causes severe diarrhea, vomiting, fever, and death.
When physician John Snow began questioning people in the neighborhood, he noticed that of the seventy-seven households infected with cholera, fifty-nine used the hand pump on Broad Street. Families that remained healthy used a water pump farther away.
Near the Broad Street well was a cesspool that contained the waste and garbage of the neighborhood. Snow believed that sewage from the cesspool had contaminated the drinking water. He begged the board of trustees of the St. James Parish to remove the handle from the pump to prevent people from collecting the contaminated water. Although no other physician agreed with Snow's assessment, the men on the board did as he advised. The handle was removed and the cases of cholera declined. Later Snow learned that the bricks lining the cesspool were indeed old and broken, and sewage had leaked into the well.
Disease Detectives Today
The same kind of detective work that Snow conducted in the 1800s is carried out today by scientists at the Centers for Disease Control and Prevention (CDC) headquartered in Atlanta, Georgia, and the Division for Emerging and Other Communicable Diseases Surveillance and Control at the World Health Organization (WHO). More properly called epidemiologists, these scientists study the spread of infectious illnesses and respond to outbreaks anywhere in the world.
They watch for the emergence of a new disease or an old microbial adversary using a network of doctors and high-tech equipment like satellites and the Internet. The WHO is continuously monitoring the World Wide Web with a customized search engine called the Global Public Health Intelligence Network, listening for rumors and reports of suspicious diseaserelated events. Online eavesdropping led to the early detection of the 2003 outbreak of SARS (severe acute respiratory syndrome).
When a suspicious event is detected or when epidemiologists are consulted by local authorities, these scientists use some of the same skills that police detectives use when trying to solve a crime. They interview the patients, their friends, and family to pinpoint the initial signs of illness. They ask patients what they may have eaten, what animals or animal products they may have come in contact with, and where they may have traveled. As each person is interviewed, patterns of the disease emerge. Are the victims all children, or are they all adults? Are they mostly male or female? Knowing when an outbreak began, who it affected, and when it ended gives epidemiologists an idea of the kind of disease that could have occurred within that time frame.
Epidemiologists also track each patient's activities to narrow down the possible source of infection and plot each incident on a map to see if there is a geographical element. They search the area for evidence of animal activity, insects, or contaminated water or food. Doctors take samples of blood or tissue and send them to their lab in Georgia, where microbiologists will identify the microbes involved in the incident.

Suspect infectious agents are examined in a lab called a biocontainment unit. There are four levels of security and safety features in the labs. The most deadly infectious agents are examined in biocontainment unit level 4, which is as airtight as a space shuttle. Air locks and a ventilation system that sucks air inward prevent dangerous bacteria or viruses from drifting out. Microbiologists suit up in astronaut-like "blue suits" complete with their own air supply. At the end of the day, the workers are decontaminated in chemical showers. The evidence found in the lab combined with the information gathered in the field will lead to the cause and hopefully the treatment of the infection.
Microbes on the Move
Epidemiologists respond to outbreaks all around the world, but today our world is more mobile than ever before, and that mobility means that microbes are on the move too. "One of the most important means of spreading diseases around the globe is air travel," 22 says David Heymann, the director of communicable diseases for the World Health Organization.
Every day, more than 500 million people travel across international borders, and tens of billions of bacteria and viruses hitch a ride. In 2003, within six months of the first reported case of SARS in China, the disease was spread by air travel to twenty-seven other countries. All the victims who came down with SARS in Toronto, Canada, could be traced directly back to one woman who had traveled from Hong Kong. And shortly after the Toronto outbreak, the World Health Organization warned travelers not to visit the city and effectively prevented the virus from spreading further.
Changing the Environment
People not only get around faster than ever before, but they change the environment more easily too. Every day, in some part of the world, whole tracts of rain forests are bulldozed, rivers are dammed, and new roads are paved into the wilderness. This disrupts the balance and distribution of plants and animals, including microbes. It may cut off a virus from its host so that the virus must seek another means of survival.
The story of Lyme disease, which causes arthritis-like aches and pains, provides an example of this process. In the 1800s settlers in Old Lyme, Connecticut, clearcut the old growth forests, which led to a decline in the deer population. A hundred years later, when the agricultural production in that area ceased, the forests returned, along with a burgeoning deer population. But the human population grew too. Housing developments in forested areas put man, deer, and microbes on a collision course.
The spirochete Borrelia burgdorferi is passed from a deer to a deer mouse by the bite of an infected deer tick. The deer and the deer mouse do not seem particularly affected by the microbe, but people are. When people started to build houses in Old Lyme, they unwittingly placed themselves in the path of the microbe and added a new host to the microbe's list.
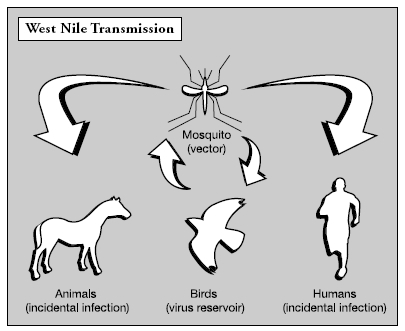
Even making more subtle changes to the landscape—such as digging pools, opening irrigation ditches, and discarding tires—create new niches for vectors, animals that are capable of carrying human disease. Insects carry about one hundred different human diseases, which are called arboviruses ( ar thropod- bo rne viruses). Topping the list are yellow fever, dengue fever, malaria, and West Nile virus.
West Nile Virus
In the summer of 1999 the New York City Health Department battled a mysterious outbreak of encephalitis (inflammation of the brain) among a group of elderly people living near LaGuardia Airport. Tests revealed that it was West Nile virus, a disease never before seen outside of the Middle East.

The virus is carried by mosquitoes that take advantage of hot, wet summers in urban and suburban areas. "West Nile is extraordinarily good at adapting to this new environment," 23 said Ian Lipkin, director of the Jerome L. and Dawn Greene Infectious Disease Laboratory at Columbia University. Mosquitoes lay infected eggs in puddles, pools, overturned toys, garbage cans, and any other place rainwater can accumulate.
West Nile usually infects birds. People living in the suburbs of Chicago, one of the most heavily hit areas, reported an eerie silence where once songbirds trilled and crows cawed. No one knows why or how it got to the United States, but this versatile virus managed to quickly jump species once it arrived. It is now known to infect dozens of bird species, as well as humans, horses, chipmunks, squirrels, raccoons, bats, rare rhinoceroses in zoos, and wild alligators. These animals are only innocent bystanders in the virus's life cycle.
In order to cause disease, a mosquito must first bite an infected bird and pick up the virus, which ends up in the digestive tract of the mosquito, where it multiplies. While other arboviruses are carried inside the gut of only one or two species of insect, the West Nile virus has been found living in thirty-six different species of mosquito. The virus spreads throughout the mosquito's body, ending up in the salivary glands. When the mosquito bites its next victim, the virus is injected into the new host along with mosquito saliva.
In the short time since West Nile virus first appeared, scientists have learned a great deal about it. The virus's ability to replicate is closely related to the weather. At 70 degrees Fahrenheit, it takes the virus three weeks to multiply to a point where it is transferable to another animal. At 80 degrees Fahrenheit, the time is shortened to two weeks, and during spells with temperatures higher than 90 degrees Fahrenheit, it takes only one week. The hotter the weather, the more infectious the disease becomes. This information is not just interesting virus trivia; it is vital data that allows health officials to predict the severity of an outbreak by monitoring the weather. If a large outbreak is predicted, then officials may spray insecticides and issue health warnings to residents in the area. But even with early warnings, the disease
is spreading. At the end of 1999, the CDC reported that sixty-two people had been infected in four states and seven people had died. Within three years, the virus had spread to forty-four states, reporting 4,156 cases of illness and 284 deaths.
Hidden Danger
Some infectious diseases are spread by animals, while others are passed directly from person to person. Some may sweep through a population like wildfire, while others lurk and linger.
In the summer of 1981, five men in Los Angeles were hospitalized with weakened immune systems and uncontrolled rare infections and tumors. Not long afterward, similar cases were reported in New York, San Francisco, and Newark, New Jersey. By the end of the year, 150 cases of the illness had been reported and thirty people were dead. This was the first slow appearance of what would later be called human immunodeficiency virus (HIV), which causes AIDS (acquired immunodeficiency syndrome). After years of study, researchers discovered that this RNA retrovirus might have made its first appearance in the human population as early as 1959, perhaps even earlier. HIV is capable of hiding out within a person's cells for up to twenty years before the symptoms of AIDS develop. Like other viruses, HIV targets one particular kind of cell, but the reason that HIV is so deadly is that it attacks the immune system's white blood cells. By entering and killing only those cells, the virus kills the cells that allow the body to protect itself against other infectious diseases.
Hiding out inside a person's cells for years is an effective way for the virus to survive. It can be passed from person to person long before any signs of illness appear. HIV can spread through having contact with blood and other bodily fluids from an infected person, engaging in sexual activity with an infected person, sharing a contaminated hypodermic needle, and
receiving a blood transfusion. It may also be passed from an infected mother to her fetus during pregnancy.
As one of the smallest viruses, measuring only .1 micron in size, HIV has caused as much devastation in the African continent as smallpox did in the New World five hundred years ago. In Zimbabwe and other African countries, one out of every five adults is infected. But the virus is also a worldwide epidemic. The WHO reported that at the end of 2003 an estimated 40 million people across the globe lived with HIV, and the disease AIDS had taken the lives of 25 million. With no vaccine and very few effective long-term treatments, AIDS continues to take the lives of 3 million people every year.
Biological Warfare and Terrorism
It would seem that the CDC and the WHO have enough on their plate just monitoring and responding to natural outbreaks of disease, but they also respond to acts of bioterrorism—the use of a biological substance like a bacteria or a virus as a weapon. Bioterrorism is a concept nearly as old as war itself. Greek and Roman armies threw dead and bloating animals into their enemy's water supplies to make them sick. In 1763 British officers gave gifts of smallpox-infected blankets to unsuspecting Native American chiefs. For decades many nations, including the United States, experimented with microbes as weapons until the ratification of the Bacteriological and Toxic Weapons Convention in 1972. But evidence suggests that some countries and terrorist groups still have active biological warfare programs.
The list of potential bacterial and viral weapons is short but deadly. The microbes most likely to be used for an attack are those that are highly lethal, easily produced in large quantities, and easily transmittable. Anthrax tops the list, because it can be collected from soil samples or illegally acquired from germ banks. It can be contracted through the skin or ingested. It attacks the body and shuts down the immune system. Inhaling anthrax is almost always fatal.
Each year the U.S. federal government responds to hundreds of anthrax hoaxes, but on October 5, 2001, it was the real thing. On that day began a series of biological

terrorist attacks in which envelopes containing high-grade anthrax were sent to addresses in Florida, New Jersey, New York, and Washington, D.C. Seventeen people were taken ill, and five people died. The attacks shut down the postal service and other government agencies for several days, costing the nation millions of dollars.
The botulin bacterium has also been used as a weapon because it produces one of the most toxic chemicals known, but it cannot be as effectively distributed. In 1984 members of the Rajneesh cult in Oregon sprinkled the bacteria on restaurant salad bars in an attempt to affect the outcome of an upcoming local election. The Oregon incident injured more than seven hundred citizens but did not cause any fatalities.
The smallpox virus is another cause for concern. When the virus was eradicated from nature, there was no need to continue the vaccination program, so today very few people have a natural immunity to fight the disease. It would spread easily through a population. In 2002, in the wake of the World Trade Center attack and the anthrax incidents, President George W. Bush announced reinstating a voluntary smallpox vaccination program for frontline health-care workers and first responders and a mandatory vaccination program for military personnel.
Investigations have uncovered that microbes like smallpox or anthrax can be obtained illegally from unregulated labs and former storehouses. No one knows how many deadly germs are available or easily obtainable, but according to the World Federation for Culture Collections, there are forty-six registered germ banks that contain anthrax, and there are more than one thousand that are not registered or regulated.
These germ banks are like microbial libraries where legitimate scientists can request specimens of certain bacteria or viruses for research purposes. They hold more than just dangerous pathogens. Germ banks also contain an assortment of other bacteria and virus cultures that are experimented with and used for more positive purposes.
Comment about this article, ask questions, or add new information about this topic: